The Rex Laboratory




3. Erythropoietin
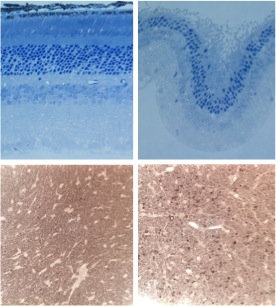
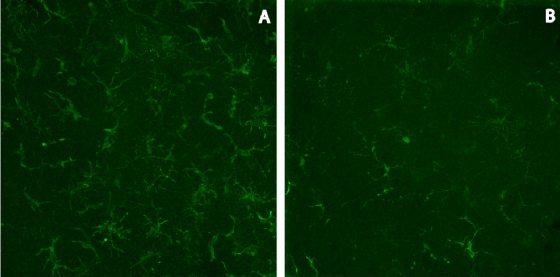
Erythropoietin (EPO) was first identified as a cytokine that blocks cell death of
red blood cell precursors resulting in an increased hematocrit. More recently it
was found to be able to block neuronal cell death in multiple models. In addition,
it can decrease oxidative stress and neuroinflammation as described in our recent
review (Figure X). Since all of these processes occur in both glaucoma and ocular
trauma we are investigating the efficacy of EPO therapy in models of these degenerations.
To avoid the increase in red blood cell production while maintaining neuroprotection
we use a mutant form of EPO that we identified, EPO-
We have achieved good success with recombinant adeno-
Research in the Rex Laboratory is split into three main areas of interest.
1. Ocular Trauma
An estimated 300,000 service members were exposed to improvised explosive devices in the recent wars in Iraq, resulting in traumatic brain injury (http://veterans.rand.org). Recently, a group of Veterans with mild traumatic brain injury due to blast exposure, who retained closed globes, were shown to have ocular pathologies including corneal abrasions, hyphemas, cataracts, corneal edema, angle recession, hemorrhage, retinal tears or detachments, macular holes, choroidal rupture, commotio retinae, and optic neuropathy (Blanch and Scott, 2009; Cockerham et al., 2011). Unfortunately, most service members and Veterans do not receive this level of examination so the prevalence of vision impairing damage is unknown. Further, since the realization that blast exposure without the presence of perforating or penetrating injury may cause permanent vision loss due to damage to the retina is new, there is a lack of animal models.
We have developed and characterized a system that directs an over-
2. Glaucoma
Glaucoma is a neurodegenerative disease of complex etiology. The underlying mechanisms
leading to retinal ganglion cell death and permanent vision loss are being actively
elucidated. We now know that Glaucoma is an axonopathy -